CMS Medicare Advantage and Medicaid Resource Hub
Discover the latest insights and proven provider data management tips for CMS compliance. Our expanding collection of resources is here to help you achieve your Medicare Advantage and Medicare-Medicaid Plan goals.
Policy Brief: CY2025 Medicare Advantage Final Rule
Get Ahead: 2025 CMS Medicare Advantage Insights. New Network Adequacy Requirements explained. Download our policy brief today.
Discover Your Opportunity, Network Build and ROI
When you’re preparing to expand your Medicare Advantage Provider Network footprint, it’s important to understand the costs and potential ROI of adding new counties. In this video, Eliza Hoffman, VP of Regional Payers, shares how she and her team can help you understand the network build effort to expand into each desired county, the potential ROI upon achieving average enrollment, and which providers to contract with to quickly and efficiently fill specialty gaps. Schedule your Complimentary Opportunity Analysis today!
Explore Our Latest Articles

NETWORK ADEQUACY AND PROVIDER DIRECTORY ACCURACY POLICY UPDATES
Just in: Network adequacy and provider directory policy updates! Stay in the know with our comprehensive update on the changes that emerged between December ’23 and February ’24. Don’t let these updates catch you off guard – read the article now.
Ghost Networks
Medicare Advantage Applications and Letters of Intent: Process and Timelines Explained
Wondering when and how to submit Letters of Intent during your Initial or Service Area Expansion application? Roxanne Butts, Client Services Consultant at Quest Analytics, walks you through the operational instructions and submission timelines.
What to Do When Your Medicare Advantage Contract is in Jeopardy
Discovering network deficiencies after submitting your HSD table to CMS can be stressful. Where should you start if you want to quickly add providers to the network? Eliza Hoffman, our VP of Regional Payers Segment, shares the answer.
Find More Videos from Quest Analytics
Learn the latest news, insights, and strategies, from the experts at Quest Analytics. Explore our collection of provider network management videos on our YouTube channel.
🔔 Subscribe Today to be the first to access new content as soon as it’s released!
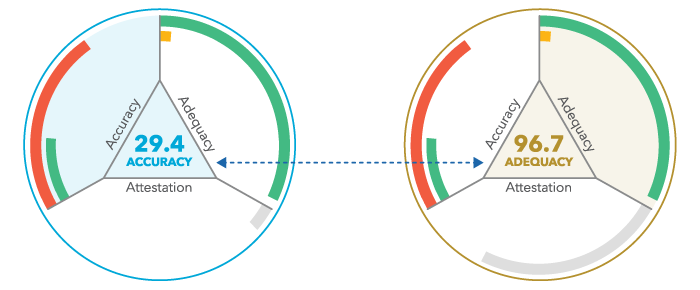
MEASURE YOUR NETWORK LIKE CMS
Ready to evaluate your provider network the same way that regulators will evaluate it? Quest Analytics delivers the answers to your test – bringing peace of mind by showing you what regulators will see when they evaluate your network. Our Medicare Advantage and Medicare-Medicaid Network Adequacy templates will reduce your compliance testing time and cost, leaving you with more time to focus on getting better insight into your data and taking action where it matters.
Provider Data Management Tips & Resources
Streamline Your Network Adequacy Exceptions
EXPEDITE YOUR PROCESS. ENHANCE YOUR EXCEPTION NARRATIVE.
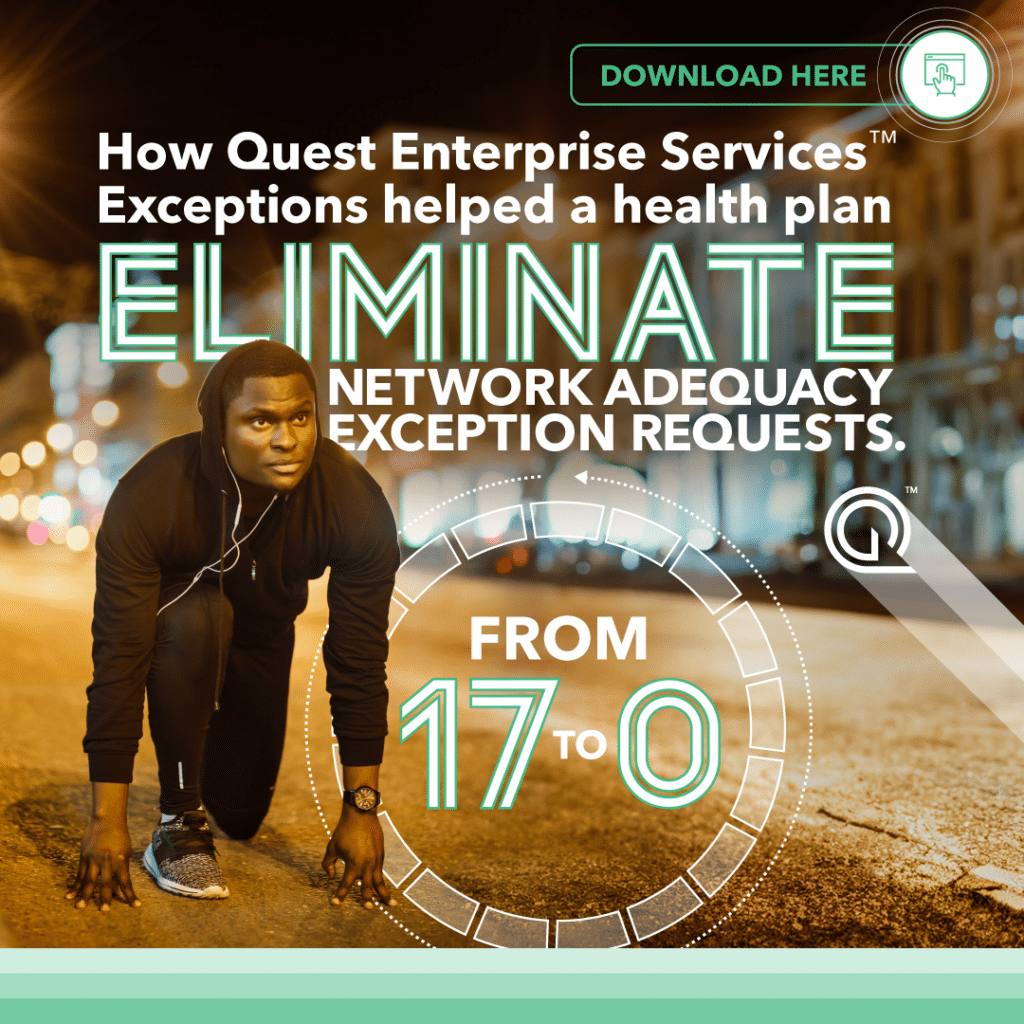
Getting a network adequacy exception request accepted is no walk in the park. This can be true whether you’re submitting to the Centers for Medicare & Medicaid Services (CMS) or a State Regulator. The Quest Enterprise ServicesTM Exceptions Package automates and simplifies your network adequacy exception request process for CMS or the State, leaving you with more time to focus on other priorities. Discover how one health plan uses the Quest Enterprise Services Exceptions Package to reduce, expedite and enhance their network exception requests.
Success Stories

Press Release
CMS EXTENDS ITS CONTRACT WITH QUEST ANALYTICS
The Centers for Medicare & Medicaid Services (CMS) has extended their contract with Quest Analytics for an additional five-year term to measure the adequacy of all Medicare Advantage Part C & D and Medicare-Medicaid Health Plans’ (MMP) provider, facility and pharmacy networks.
SCHEDULE YOUR COMPLIMENTARY NETWORK ASSESSMENT
Interested in discovering how we can assist you with your service area expansion and network adequacy goals? Schedule your complimentary network assessment with a Quest AnalyticsTM expert today.