QHP Certification and Network Adequacy Review Timeline
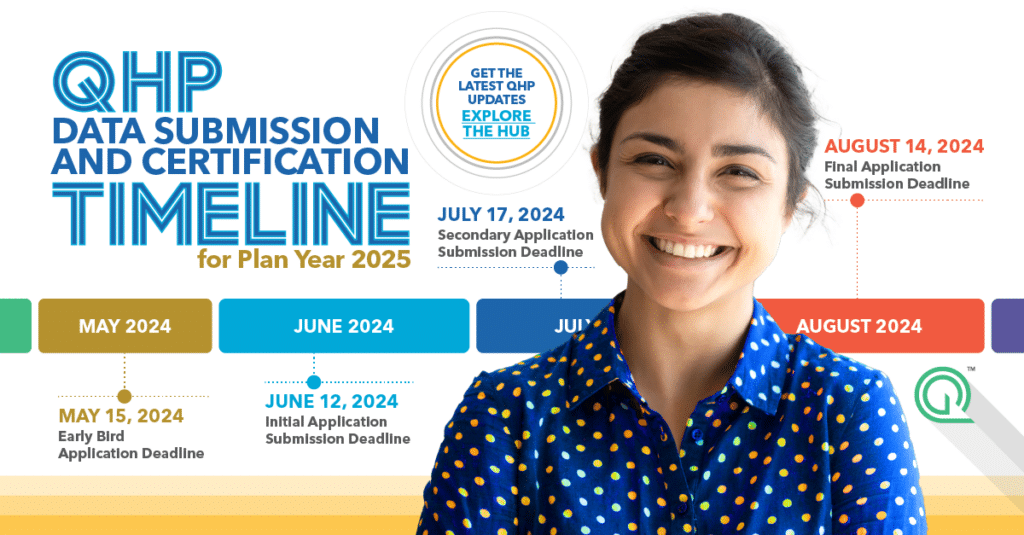
Who doesn’t love a good calendar? We know we do. Whether you’re deep into network adequacy updates or juggling deadlines left and right, we’ve got your back. Our handy calendar lays out the crucial submission dates for Qualified Health Plan (QHP) issuers on Federally-facilitated Exchanges. As a bonus, we’ll keep it updated for you! Go ahead and […]
Network Adequacy and Provider Directory Accuracy Policy Updates

Now that 2024 is fully underway, we’d like to bring you up to speed on the network adequacy and provider directory policy updates that emerged between December 2023 and February 2024. Federal Policy Updates CMS Issues Request for Information on Medicare Advantage Data The Centers for Medicare & Medicaid Services (CMS) opened the year with […]
CMS Corrective Action Plans: What Medicare Advantage Organizations Need to Know

The Centers for Medicare & Medicaid Services (CMS) turned things up a notch with new provider directory requirements last year, and now they’re doubling down with Corrective Action Plan requests for Medicare Advantage (MA) Organizations that aren’t playing by the rules. We’re breaking down the latest news about the added provider directory requirements and Corrective […]
CMS Changes the Network Adequacy Application Process for Medicare Advantage Organizations

If you’re involved with compliance, market expansion, or provider recruitment for a Medicare Advantage (MA) Organization, listen up! As organizations seek to either enter the Medicare Advantage market or expand their service areas, understanding these changes is paramount to achieving compliance and securing approval. Network Adequacy Reviews for Initial or Service Area Expansion Applications MA […]
Network Adequacy and Provider Directory Accuracy Policy Updates

What’s the latest news on network adequacy and provider directory accuracy? Here’s what took place in November. Download Article Federal Policy Updates Proposed Rule: 2025 Medicare Advantage Program New Mental Health Facility-Specialty Type and Network Adequacy Exceptions The Centers for Medicare & Medicaid Services (CMS) proposed changes to the Medicare Advantage program for the contract […]
The Requiring Enhanced & Accurate Lists of Health Providers Act

Are enrollees receiving the healthcare services they were promised? Inaccurate provider directories and ghost networks have been longstanding concerns in the healthcare industry, particularly with mental health services. Recognizing the need for improvement, lawmakers have introduced new legislation to address inaccurate data and help seniors receive the care they purchased. The Requiring Enhanced & Accurate Lists […]
Network Adequacy and Provider Directory Accuracy Policy Updates

Looking for the latest updates on network adequacy and provider directory health policies? You’ve come to the right place. Let’s dive into the latest federal and state policy developments. Download Article Federal Policy Updates Regulators and policymakers are dedicated to strengthening the oversight process for Medicare Advantage, Marketplace, and Medicaid Health Plans, both at the […]
What You Need to Know About QHP Certification
Staying on top of all the latest updates in the industry can be a real challenge. That’s why we’re here to break down everything you need to know about the Qualified Health Plan (QHP) certification and network adequacy compliance. Grab your favorite beverage and get ready to dive into the world of QHP certification and […]
Mark Your Calendars: Important Medicare-Medicaid Plan Network Submission Coming Up
Time flies when you’re managing a Medicare-Medicaid Plan (MMP) provider network. Before you know it, the network submission deadline is just around the corner—and we’re here to ensure your success. Get ready to take note of the important details! Network Submission Due Date Reminder Key Dates and Times Let’s dive straight into the specifics. The […]
Four Ways Regulators Prioritize Health Equity into Network Adequacy
In the pursuit of high-quality healthcare, it is essential to go beyond network adequacy metrics and prioritize health equity. In a conversation between Scott Westover, SVP of Network and Regulatory Strategy at Quest Analytics, Michael Conway, Colorado Insurance Commissioner, and Grace Arnold, Minnesota Department of Commerce Commissioner, we learned how these leaders are working together […]