The Role of Adequate Health Networks in the Marketplace
Quest Analytics® is hosting leadership from The CMS Center for Consumer Information and Insurance Oversight (CCIIO) for a conversation about network adequacy requirements and standards. CCIIO develops and implements the provider network standards health insurance plans must meet to participate in the Federally-facilitated Exchanges (FFEs). This discussion will address various topics focusing on requirements introduced […]
Quest Analytics Regulator Exclusive Webinar
Regulator Strategies for Improving Provider Directory Accuracy, Eliminating Ghost Providers and Encouraging Provider Engagement Why attend: Understand the challenges and solutions in maintaining accurate provider directories. Learn about the transition from static reports to dynamic claims analysis for identifying active providers. Discover the importance of accurate data for legislative compliance and member services. Explore the […]
Bright Spots In Healthcare Podcast: Differentiating Your Health Plan: Reimagining Your Provider Network Strategy

Watch Now!
Strategies for Incorporating Telehealth Network Adequacy Credits
Facing the Realities of Provider Data Challenges to Improve Outcomes
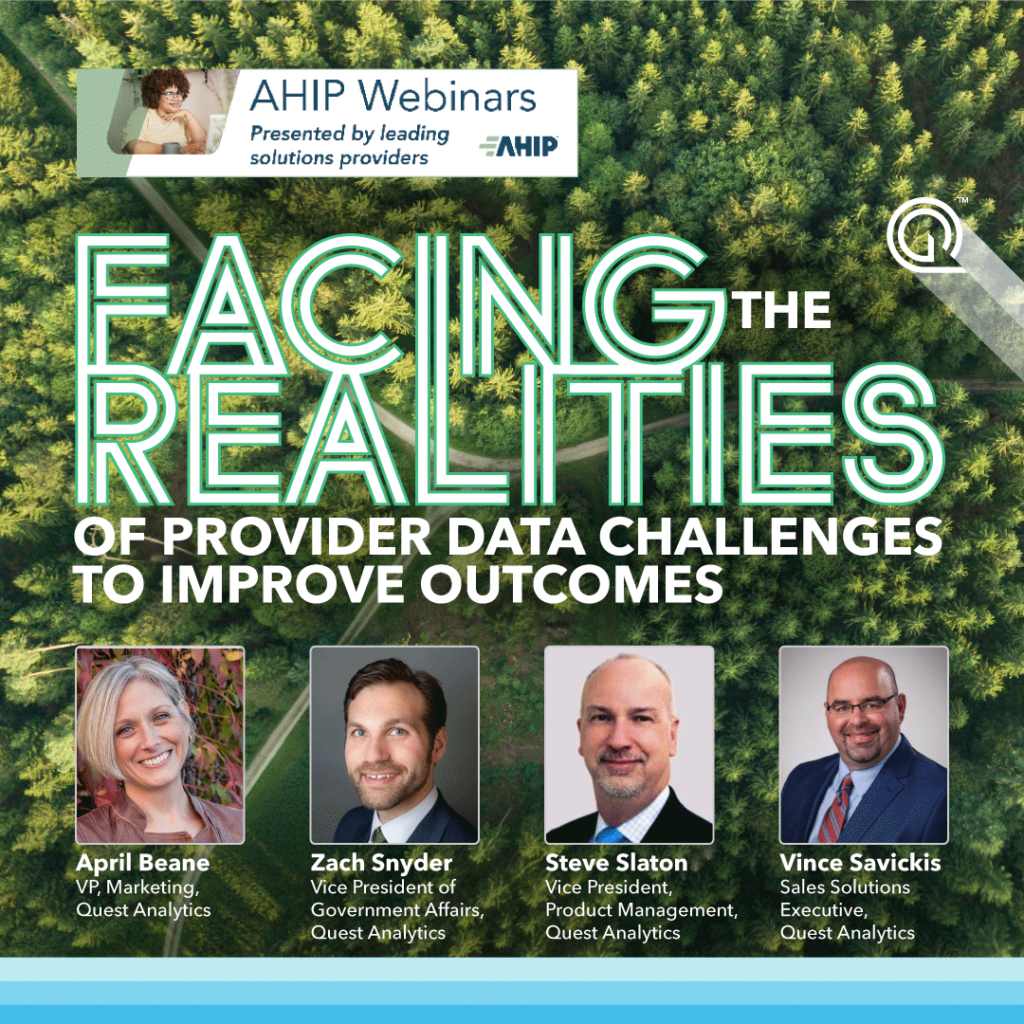
Watch On-Demand
Quest Analytics Web Learning Series
Quest Analytics Web Learning Series-November
Quest Analytics Web Learning Series-October
Quest Analytics Web Learning Series-September
Quest Analytics Web Learning Series-August