QHP MARKETPLACE RESOURCES
Essential resources for issuers applying for QHP Certification to participate in the Marketplaces. Explore our growing library to find the latest news, tips, and support.
PY2025 QHP Certification Marketplace Final Rule
Big changes! Discover the latest PY2025 & PY2026 network adequacy requirements for QHP certification in state and federal Marketplaces.
Executive Summary: New Rules for PY2025 QHP Certification
Be Ready for Network Adequacy and QHP Application Changes Understanding the New QHP Certification Process Big changes are just around the corner! Network adequacy requirements for Qualified Health Plan (QHP)...
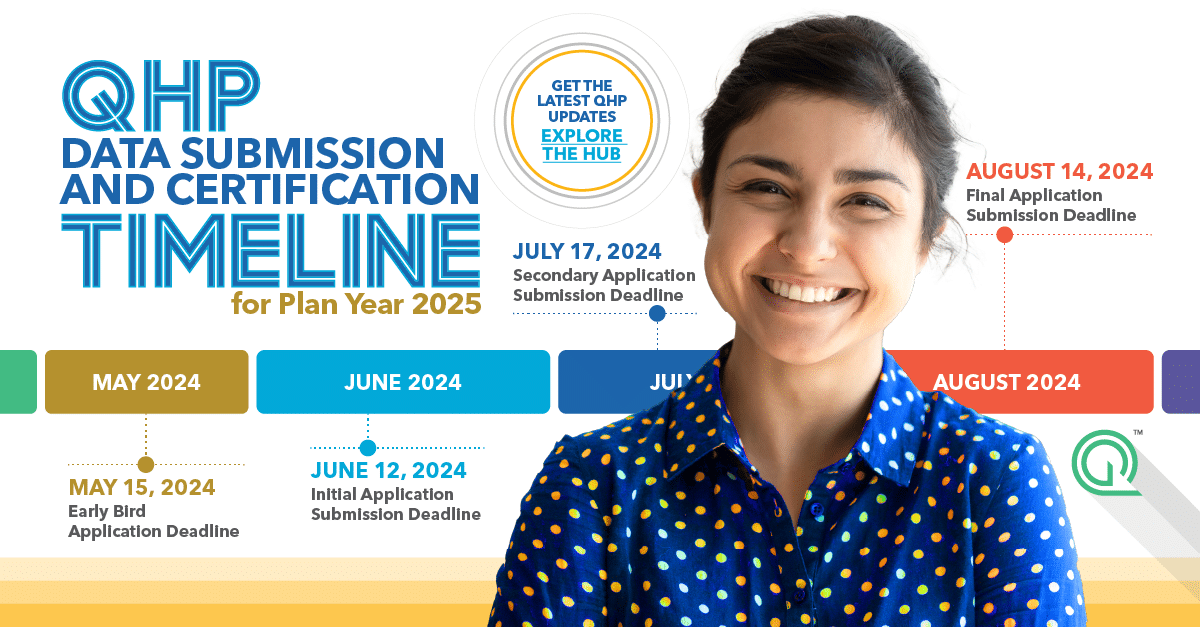
QHP Certification and Network Adequacy Review Timeline
Who doesn’t love a good calendar? We know we do. Whether you’re deep into network adequacy updates or juggling deadlines left and right, we’ve got your back. Our handy calendar...
What You Need to Know About QHP Certification
Staying on top of all the latest updates in the industry can be a real challenge. That’s why we’re here to break down everything you need to know about the...
Tips for QHP Issuers: Completing the Network Adequacy Template
Successfully Submit Your Network Adequacy Data Get ahead in your QHP certification by providing the correct information. Take advantage of these six tips to successfully submit your data using the...

Network Adequacy and Provider Directory Accuracy Policy Updates
Just in: Network adequacy and provider directory policy updates! Stay in the know with our comprehensive update on the changes that emerged between December ’23 and February ’24. Don’t let these updates catch you off guard – read the article now.
Find resources, webinars, guides, and expert advice to help you stay compliant and ahead of the competition.
Provider Data Management Insights and Downloadables
Complimentary Strategy Session
Compliance isn’t our name, but it sure is our game! Learn how we can assist your efforts to make your provider data accurate and network adequate. Book a complimentary strategy session with a Quest Analytics expert to get started on your quest for success.